19 August 2025
The Malaghan Institute has been awarded three Health Research Council grants, totalling $7.4M over five years, to improve cancer immunotherapies, protect vulnerable populations from measles outbreaks and investigate new therapeutic targets for eczema.
From left: Dr Rachel Perret, Professor Ian Hermans, Dr Sotaro Ochiai
Director Professor Kjesten Wiig says receiving three major grants from the Health Research Council at a time of heightened funding constraints is significant and recognises the calibre and relevance of the Malaghan Institute’s science.
“These investments not only reflect confidence in the Malaghan’s research across cancer, allergic and infectious diseases, but also the real-world impact of our work on the health of New Zealanders.”
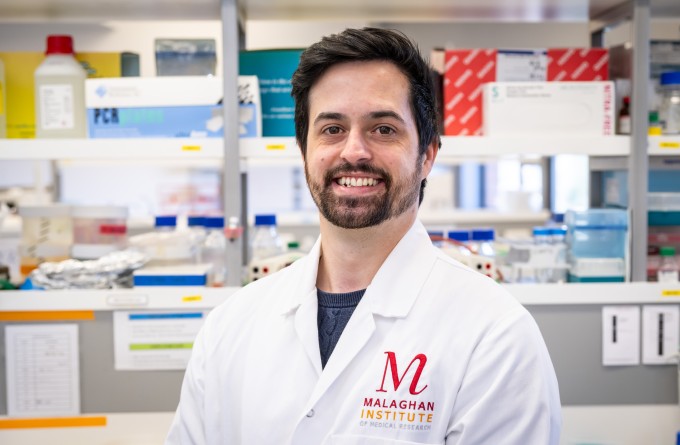
Faster CARs: Overcoming exhaustion to enhance cancer immunotherapies
Building on the Malaghan’s ground-breaking CAR T-cell programme, the Perret team in the Malaghan’s Weinkove Laboratory has recieved a $1.2 million project grant over three years to improve on this life-saving treatment.
“In Aotearoa's first CAR T-cell trial, our novel CAR T-cell therapy has shown promising safety and efficacy in people with relapsed lymphomas,” says Dr Rachel Perret. “However, a known limitation of CAR T-cell therapies is that in some cases, cancers fail to respond, or relapse. This may be due to exhaustion of CAR T-cells during manufacture or inside the patient, due to a immunosuppressive environment around the tumour.”
Cells, like people, can become exhausted if overworked or overstimulated, becoming less and less able to perform. However, unlike people, CAR T-cells can be tweaked to block the genes that signal this exhaustion, allowing them to continue fighting cancer for longer – which should also improve patient outcomes.
“This project will re-engineer CAR T-cells to silence genes linked to exhaustion and re-develop CAR T-cell manufacturing processes to enhance CAR T- cell fitness and shorten manufacturing times,” says Dr Perret. “We expect the results to be applicable to many cancer types, and to be readily translated for the benefit of New Zealanders within our CAR T-cell clinical trial programme.”
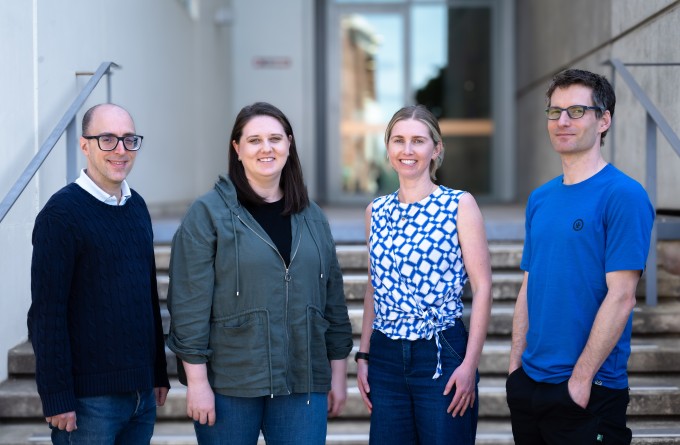
Providing equal protection for everyone against measles
Herd immunity is how we as a population protect those who are immunocompromised or otherwise unable to get vaccinated (such as very young infants) against potentially life-threatening viruses like measles. When enough of the population are vaccinated (over 95% in the case of measles), this herd immunity effectively prevents viruses from spreading to our most vulnerable whānau.
“While the current measles, mumps and rubella (MMR) vaccine is highly effective at protecting vaccinated individuals against these viruses, current vaccination rates are not high enough to provide this essential herd immunity to protect those who cannot be vaccinated,” says paediatric immunologist Dr Kuang Hsiao from Waipapa Taumata Rau, University of Auckland, who is part of the research team.
The MMR vaccine cannot be used in people with severely impaired immune systems and is not recommended in pregnant people. Also, MMR is less effective in infants, so is not routinely recommended before 12 months of age. In addition, Māori and Pacific communities are overrepresented among these vulnerable groups.
For these populations, alternate protective options are required to prevent a measles outbreak.
“Evidence has shown that mRNA-based vaccines can be effective in these vulnerable individuals,” says the Malaghan’s Professor Ian Hermans. “With an international team involving clinicians, immunologists and Māori and Pacific researchers, we will develop an mRNA-based measles vaccine to give to vulnerable individuals in the event of an outbreak.”
The research has been awarded an HRC Programme Grant, worth $5M over five years, and will bring together multiple organisations including the Malaghan, representing diverse areas of expertise and combining both fundamental research and public health.
“As part of this work, we will explore with Māori and Pacific communities’ perceptions and beliefs about mRNA-based vaccines to support equitable access to the vaccine,” says Dr Hermans.
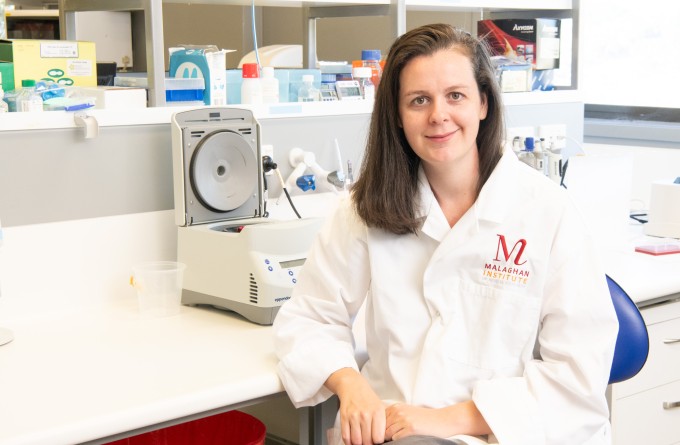
Investigating novel treatment targets for atopic dermatitis
Atopic dermatitis, or eczema, is a chronic skin allergic disease that affects a significant proportion of New Zealand’s population. The disease can have a significant negative impact on a person’s livelihood with symptoms varying from persistent itchiness, redness, dryness and inflammation. Current treatment options are largely immunosuppressants such as corticosteroids, which can cause side effects. While these treatments can help manage symptoms there are currently no effective therapies to prevent the disease from developing and relapsing.
At the cellular level, one hallmark of atopic dermatitis is the chronic infiltration and persistence of immune cells called tissue resident memory T-cells. Normally, these cells are vital for protecting the skin from invading pathogens, but for individuals with atopic dermatitis these cells also contribute to the disease by promoting recurring inflammation even after the allergen has been cleared from the skin.
The project, which has been awarded $1.2 million over three years, will be led by Dr Sotaro Ochiai, a Senior Research Fellow in the Ronchese Laboratory. The team will focus on better understanding these tissue resident memory T-cells identifying key genes and biological pathways that are essential for the establishment and maintenance of these cells in the skin.
“By understanding these mechanisms, we aim to identify new therapeutic targets to disrupt tissue resident memory T-cell survival or function and improve quality of life for those affected by this persistent and distressing condition,” says Dr Ochiai.
Related articles

NZ-UK research deepens understanding of germinal centres for better vaccine design
27 January 2026
How a quirk of the immune system may play a big role in protecting us from disease
18 December 2025

Dr Kerry Hilligan awarded Sir Charles Hercus Health Research Fellowship
2 December 2025
The nose knows: new research explores next generation of nasal vaccines
2 December 2025

Tracking the journey of the shapeshifting bacteria behind stomach cancer
19 November 2025
Marsden funding to drive discovery and innovation in cancer, allergy and infectious disease research
5 November 2025
