29 October 2025
Immune checkpoint inhibitors have revolutionised cancer treatment in recent years, offering more options for fighting this devastating disease. A type of immunotherapy, immune checkpoint inhibitors work by blocking signals that trigger the ‘off switch’ on T-cells – allowing these cancer-killing immune cells to keep fighting cancer for longer.
Professor Ian Hermans (left) and Dr Regan Fu.
The immune system is all about balance. For powerful cancer-killing immune cells like T-cells, having ‘off switches’ to halt their activity is just as important as ‘on switches’, to prevent other innocent cells getting caught in the crossfire. We call these switches ‘checkpoints’ – proteins that help keep T-cell activity in check.
However, cancers cells have evolved to take advantage of this protective mechanism, sending their own chemical signals to activate these checkpoints and turn off T-cells prematurely. Checkpoint inhibitors do exactly as advertised – they stop the stop signal – a biological double negative that has the positive outcome of keeping T-cells activated for longer – a game-changer in the fight against cancer.
Yet despite the widespread success of immune checkpoint inhibitors, unfortunately many patients don’t respond to the therapy. This may be because the microenvironment surrounding and within solid tumours has evolved to be incredibly effective at suppressing T-cell and other immune cell activity. This means that even with their off switch turned ‘off’ the T-cells can’t do much.
One strategy to overcome this is to reset the microenvironment inside tumours by introducing immune-stimulating molecules designed to activate within solid tumours. By giving the immune system this shake up at these very specific sites, it may be possible to overcome this suppressive environment, allowing the T-cells ‘unleashed’ by checkpoint inhibitors to work as intended. As part of a long-standing collaboration, the University of Auckland’s Auckland Cancer Society Research Centre (ACSRC) and the Malaghan Institute’s Hermans Lab are investigating just this opportunity.
Resetting the tumour microenvironment
The Achilles’ heel of many immunotherapies is that immune cells must be at the site of the disease to act. Even with the best checkpoint inhibitors, if the T-cells can’t access all the cancer cells, they can’t do their job.
Solid tumours can employ a number of insidious tactics to create a hostile environment to T-cells, preventing these immune cells getting in and doing their job. Not only do these dense masses of cancerous cells create physical barriers to prevent infiltration by immune cells, they can produce immune-suppressive molecules, create toxic metabolic byproducts and recruit other cells that further subdue immune cell activity.
“For immunotherapies to be effective for solid tumours, we need strategies to overcome the tumour microenvironment.”
“We call this the ‘cycle of suppression,’ a selfreinforcing cycle designed to evade and disarm the immune system,” says Professor Ian Hermans. “For immunotherapies to be effective for solid tumours, we need strategies to overcome the tumour microenvironment.”
For decades, researchers at the ACSRC have been perfecting the design of drugs that are selectively activated within solid tumours. Now, in collaboration with the Hermans Lab, this concept is being applied to an immune-stimulating setting. When activated inside the tumour, the drug will ‘reset’ the tumour microenvironment to be less suppressive, giving T-cells the chance to infiltrate the tumour to do their job. Add checkpoint inhibitors to the mix, and you potentially have a powerful cancer-killing combination.
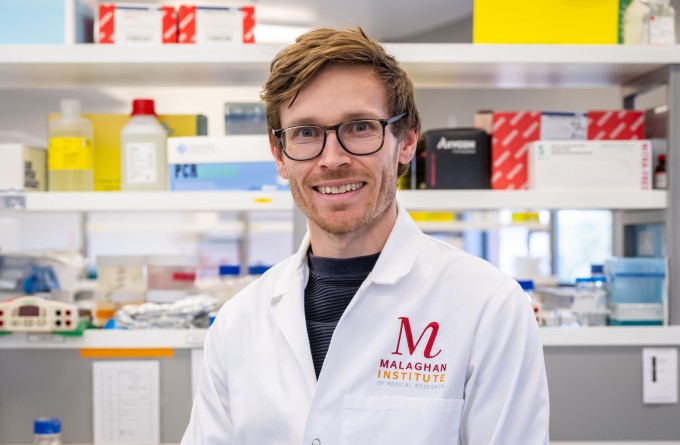
“Our earlier work on this project has been on designing and manufacturing a number of immunestimulant drugs that activate within solid tumours,” says Malaghan Institute postdoctoral researcher Dr Regan Fu. “Now, we have a number of promising drug designs that we are refining in preclinical studies to select a lead drug design for clinical studies.”
With a recent funding boost from the Ministry of Business, Innovation and Employment’s Endeavour Fund, the team aims to select a lead that works most effectively with immune checkpoint inhibitors, with the goal of generating robust data that attracts investment to a run phase 1 safety clinical trial.
“We hope the scientific data generated will take our immunooncology product into first-inhuman studies, with the ultimate goal of improving lung cancer treatment outcomes in Aotearoa New Zealand,” says Prof Hermans.
Beyond the scope of lung cancer
Immune checkpoint inhibitors are used to treat a range of cancers types around the world. In New Zealand this includes some lung cancers, melanoma, breast cancer, and colorectal cancer. Dr Fu says that while the current focus of this collaboration is on improving checkpoint inhibitors for lung cancer, there is wider potential for this research to reach more patients.
“Immune-suppression in solid tumours is common across many different cancers, so there may be an option for this product we’re working on to apply in other cancer types where checkpoint inhibitors are already in routine use in New Zealand in the future.”
Related articles

CAR T-cell therapy: 5-part video series
25 February 2026

Momentum is everything: advancing CAR T-cell research for future trials and treatments
25 February 2026

Tracking the journey of the shapeshifting bacteria behind stomach cancer
19 November 2025
Marsden funding to drive discovery and innovation in cancer, allergy and infectious disease research
5 November 2025
Eradicating H. Pylori bacterial infection to reduce stomach cancer
30 October 2025

Developing next generation CAR T-cell therapies for more equitable cancer care
30 October 2025
