24 September 2025
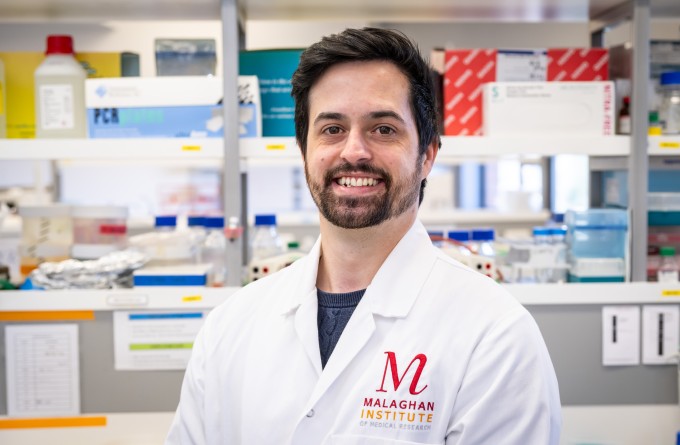
Dr Brigitta Mester, the Malaghan Institute’s R&D and process development manager, has been at the heart of bringing New Zealand’s first CAR T-cell clinical trials to life, doing the groundwork to ensure the therapy meets world-class standards and safety.

Brigitta’s office for many years was nestled at the end of the first-floor corridor opposite the most tightly controlled labs at the institute. These labs contain machines that look like they’ve come straight out of a sci-fi novel.
These sleek, pearly capsules, aptly named Cocoons, gently rock newly formed CAR T-cells from side to side, nurturing them and creating the optimal conditions for them to grow.
Safeguarded by layers of automation and quality control, each Cocoon is designed to reprogramme a patient’s own immune cells into a cancer therapy, personalised just for them. For these patients, many of whom have exhausted every other treatment for their blood cancer, the cells are a last chance.
The Malaghan’s ENABLE CAR T-cell clinical trial programme, now in phase 2, represents the culmination of monumental effort by many. Brigitta has been pivotal at every step of the Malaghan Institute’s journey to bring this revolutionary new cancer therapy to New Zealanders.
“When the Malaghan Institute first set out to run New Zealand’s inaugural CAR T-cell clinical trial, the facilities looked very different,” says Brigitta.
“There were no sleek machines, no automated systems and no shortcuts. It has taken literal blood, sweat and tears from Malaghan staff to make New Zealand’s first CAR T-cell trials a reality.”
Brigitta is the Malaghan’s resident GMP specialist.
“GMP stands for good manufacturing practice. It’s an international standard laid out by the World Health Organization which aims to make manufacturing medicines as safe as possible for humans,” explains Brigitta.
“It encompasses everything related to how you make a high-quality product intended for human consumption, from the cleanliness and airflow of the lab to how clearly and consistently you label different components to avoid mix-ups.”
Brigitta had already been involved in setting up GMP facilities for Malaghan’s previous clinical trial, testing a therapy for melanoma.
“We were just wrapping up the MELVAC trial when we got word that the Malaghan might be testing a new promising CAR T-cell therapy. I'd never heard of CAR T-cells before. I was asked to investigate the regulatory landscape of this therapy before we agreed to undertake the clinical trials for this new therapy.”
Brigitta and the team pored over all available documentation on this brand-new therapy. The more they read, the more excited they became.
CAR T-cell therapy works by taking the patient’s immune cells and modifying them genetically so they can recognise the cancer they are treating. These genetically modified cells are then multiplied so there are enough to infuse back into the patient to hunt down and destroy malignant cells.
Showing huge potential as the future of cancer therapy, the small team of dedicated scientists involved in evaluating the possibility of running a CAR T-cell trial saw that this could usher in a new era of treating blood cancers in New Zealand. However, they also knew that the challenge of building New Zealand's first CAR T-cell therapy trial from scratch would be Herculean.
There was no playbook and no existing infrastructure.
“If that wasn’t enough of a challenge, we were doing this on a shoestring budget with just 2.5 lab scientists,” says Brigitta.
“I just knew from the moment I heard about this trial and the potential it held that I wanted to be part of it.”
The early days were relentless.
“We started by setting up a dedicated GMP production suite, suitable for manufacturing not just the CAR T-cells, but some of the required reagents as well. We did a lot of scrubbing in those early days. Every inch of the lab, including the air itself, had to be clean. We spent a lot of early mornings and late nights setting up the suite, cleaning, testing sterility, installing specialised equipment.”
Every procedure had to be written from scratch and the paperwork piled up fast. In Brigitta’s office, filing cabinets stretch from floor to ceiling, were packed full with the documentation she and the team produced to meet regulatory requirements.
Then came the testing. Before patient samples could be used, Malaghan staff were asked for blood donations.
“We could not use our own, because if we came into contact with any genetically modified cells specific to us, it could get risky. So we had to ask non-lab staff if they might volunteer. Everyone was eager to help, but our team did get the reputation of being vampires who needed a continuous supply of blood,” laughs Brigitta.
“CAR T-cells are unlike conventional one-size-fits-all drugs. These are living cells that are carefully tailored to the individual.”
Each patient’s cells had to be grown isolated from any other cells to avoid contamination, with complete cleaning of the lab between patient runs.
“We would modify and grow cells for each patient. Feeding them, encouraging them, at times, pleading with them to grow and be healthy,” Brigitta says.
“We knew what these cells represented, a last hope for patients who had exhausted all available treatments for their blood cancer.”
It was a very different kind of trial to the ones Brigitta had worked on before.
“Previously success took the form of complicated graphs showing specific immune cell activity, but for this trial it was black and white: patient survival. The result was tangible. Depending on the outcome, our team was either energised or deeply shaken. Either way, it made us work harder for these patients.”
“Our work is enabling this revolutionary new treatment to be a reality, while paving the way for future therapies like it. We are getting closer every day.”
Over time, the process evolved. Manual work, though meticulous, was not sustainable. The Malaghan worked with Lonza to automate key steps in CAR T manufacture, using specialised machines, with a customised manufacturing protocol to emulate every step of the original manual process.
“We realised manual production wasn’t scalable, so we looked for options to automate. We are trying to automate more parts of the process so we can treat more patients while increasing the likelihood of getting a standardised product every time.”

Cocoons which automate CAR T-cell production.
This leap in capability paved the way for BioOra Limited, a spin-out company incubated at the Malaghan, set up to take CAR T-cell therapy beyond the trial stage. BioOra is making plans to build a large facility in Christchurch that will allow New Zealand to meet patient demand while maintaining the strict quality controls that Brigitta and other members of the team pioneered.
For Brigitta, the work has always been more than just a technical challenge. She grew up in Hungary and first dreamed of becoming a scientist after reading Born Free, Joy Adamson’s book about raising and rewilding a lion cub.
She arrived in New Zealand more than twenty years ago, first working at AgResearch before joining the Malaghan. While working for the institute, she also completed a PhD in cell and molecular biology at Victoria University of Wellington where she conducted research on reproductive physiology.
“I just knew from the moment I heard about this trial and the potential it held that I wanted to be part of it. I wanted this therapy to be available in this corner of the world for those who need it.”
With the phase 2 trial well underway and sights set on it being a licenced CAR T-cell therapy that is delivered through New Zealand’s healthcare system, that vision feels closer to reality.
Meanwhile, the Malaghan continues to expand its CAR T-cell research programme, which could have applications to other cancers, such as myeloma, or to autoimmune diseases.
What began as a pipedream has become something tangible. The blood, sweat and scrubbing have given way to gleaming machines, but the spirit that carried the programme this far remains the same.
“It has been a huge undertaking. Our work is enabling this revolutionary new treatment to be a reality, while paving the way for future therapies like it. We are getting closer every day.”
Related articles

CAR T-cell therapy: 5-part video series
25 February 2026

Momentum is everything: advancing CAR T-cell research for future trials and treatments
25 February 2026

A ground-breaking cancer treatment is within reach – but only if New Zealand acts now
12 February 2026
Homegrown Hope - Stuff's series on CAR T-cell therapy
11 February 2026
How a quirk of the immune system may play a big role in protecting us from disease
18 December 2025

Tracking the journey of the shapeshifting bacteria behind stomach cancer
19 November 2025
