The goal of the Hermans Laboratory is to investigate immune-based strategies to prevent or treat disease.
The use of vaccines to prevent infection has been a major advance in human health, but it is now clear that strategies to induce immune responses can also be used as a form of therapy for chronic diseases. The Hermans Laboratory has spent several years studying the cellular interactions required to elicit effective immune responses, with a focus on stimulating T-cells, a type of immune cell that can selectively kill infected or malignant cells.
The network of cellular interactions required to activate T cells includes dendritic cells, which provide the primary molecular signals needed to stimulate T cell function, and other less well-known cells, such as innate like T cells, that have the ability to influence the function of dendritic cells. Using this information, the Hermans Laboratory have worked closely with chemists to identify compounds that provoke the required sequence of cellular events to drive specific T cell responses. This has led to new vaccine designs, including mRNA-based vaccines, that induce long-lasting T cell responses in the liver. These vaccines could be used for liver-associated diseases like malaria and hepatitis, as well as liver cancer. In related work, the group is involved in developing new drugs that make solid tumours more likely to be targeted by T cells.
To conduct this work the Hermans Laboratory works closely with internationally renowned chemists and immunologists, and has close links with international groups to test new concepts in relevant models of infection and cancer.
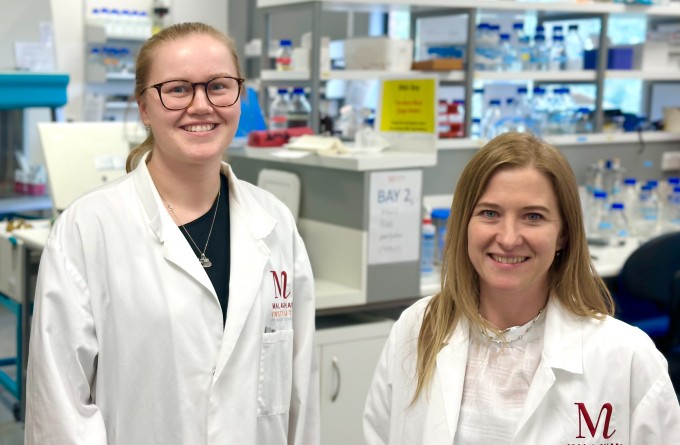
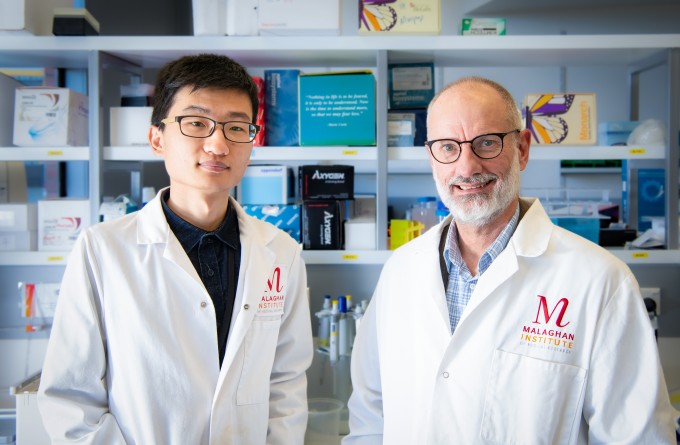
Senior Research Officers: Kathryn Farrand, Ching Wen Tang
Research Officers: John Mamum
PhD Students: Hannah Boswell, Kaitlin Buick, Jarem Wylie
Research areas
- Cancer immunotherapy
- Infectious Disease
- Vaccine design
Research projects
- Development of mRNA vaccines for cancer and infectious diseases and cancer
- Developing drugs that help immune cells eliminate solid tumours
Collaborations
Featured articles
Scientific breakthrough harnesses mRNA technology to develop powerful malaria vaccine
21 July 2023
Stopping infections at the door – designing vaccines that target immune cells in the mucosa
19 April 2023
New funding will boost RNA research into vaccines and other healthcare treatments
22 March 2023
Lung cancer immunotherapy collaboration tackling health inequities in Aotearoa
29 August 2022
Featured publications
Ganley M, Holz LE, Minnell JJ, de Menezes MN, Burn OK, Poa KCY, Draper SL, English K, Chan STS, Anderson RJ, Compton BJ, Marshall AJ, Cozijnsen A, Chua YC, Ge Z, Farrand KJ, Mamum JC, Xu C, Cockburn IA, Yui K, Bertolino P, Gras S, Le Nours J, Rossjohn J, Fernandez-Ruiz D, McFadden GI, Ackerley DF, Painter GF, Hermans IF, Heath WR.mRNA vaccine against malaria tailored for liver-resident memory T cells. Nat Immunol. 2023 Sep;24(9):1487-1498. doi: 10.1038/s41590-023-01562-6. Epub 2023 Jul 20.PMID: 37474653
Holz LE, Chua YC, de Menezes MN, Anderson RJ, Draper SL, Compton BJ, Chan STS, Mathew J, Li J, Kedzierski L, Wang Z, Beattie L, Enders MH, Ghilas S, May R, Steiner TM, Lange J, Fernandez-Ruiz D, Valencia-Hernandez AM, Osmond TL, Farrand KJ, Seneviratna R, Almeida CF, Tullett KM, Bertolino P, Bowen DG, Cozijnsen A, Mollard V, McFadden GI, Caminschi I, Lahoud MH, Kedzierska K, Turner SJ, Godfrey DI, Hermans IF, Painter GF, Heath WR (2020). Glycolipid-peptide vaccination induces liver-resident memory CD8+ T cells that protect against rodent malaria. Sci Immunol. 5(48):eaaz8035
Anderson RJ, Compton BJ, Tang C, Authier-Hall A, Hayman CM, Swinerd GW, Kowalczyk R, Harris P, Brimble MA, Larsen DS, Gasser O, Weinkove R, Hermans IF, Painter GF. (2015). NKT Cell-Dependent Glycolipid-Peptide Vaccines with Potent Anti-tumour Activity. Chem. Sci.
Anderson RJ, Tang C, Daniels NJ, Compton BJ, Hayman CM, Johnston KA, Knight DA, Gasser O, Poyntz HC, Ferguson PM, Larsen DS, Ronchese F, Painter GF, Hermans, IF. (2014). A self-adjuvanting vaccine induces cytotoxic T lymphocytes that suppress allergy. Nat Chem Biol