8 February 2024
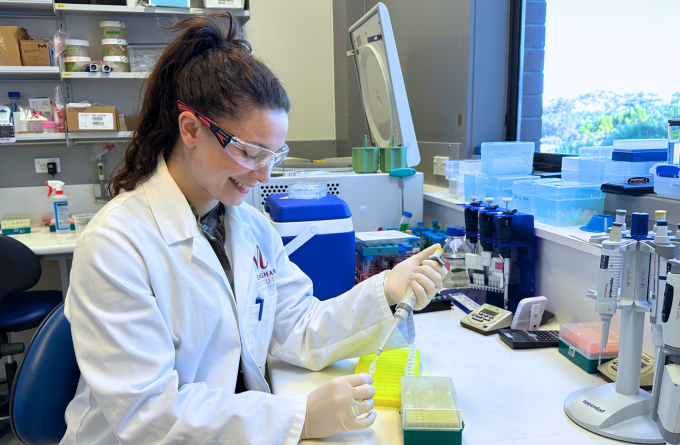
Kate Maclean is a clinical researcher in the Le Gros laboratory at the Malaghan Institute who will soon be applying her expertise in human hookworm to human bacteria, with the aim of reducing the incidence of stomach cancer in New Zealand.
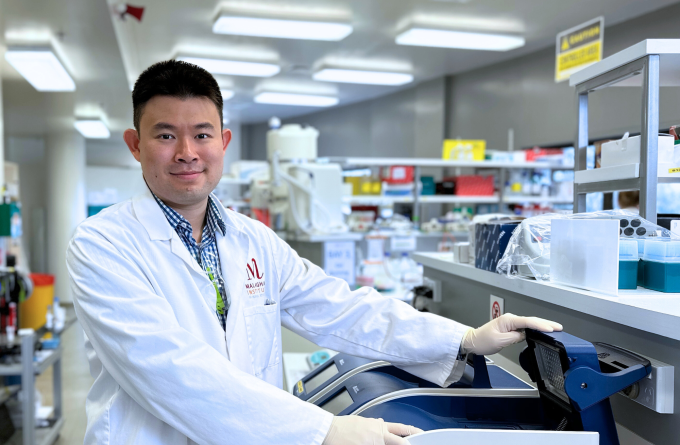
The Le Gros lab is embarking on new clinical research led by Dr Tom Mules across cancer biology and infectious disease. Collaborating with Dr Stephen Inns, a University of Otago gastroenterologist working at Hutt Hospital, the project aims to develop preventative measures for stomach cancer through early detection of antibiotic resistance to H. pylori bacterial infection in patients.
“This is quite a new avenue of research for the Malaghan Institute so I’m very excited to be working on it,” says Kate.
The focus of the research are bacteria called Helicobacter pylori or H. pylori which infect the cells of the stomach lining. Usually contracted orally, H. pylori causes gastritis, or inflammation of the stomach lining. Left untreated, the inflammation can become chronic leading to tissue damage and ulcers. This environment increases the probability of mutations in stomach cells which can cause uncontrolled cell replication and eventually stomach cancer.
“There are different strains of H. pylori bacteria, some of which are more likely to result in the development of stomach cancer,” says Kate.
Significant disparities exist in the rates of stomach cancer among Māori and Pacific populations in New Zealand, who have three to six times higher rates compared to New Zealand Europeans.
“These ethnic inequalities in stomach cancer rates predominantly stem from the higher prevalence of H. pyloriinfection among Māori and Pasifika communities due to socioeconomic factors. Additionally, Māori and Pasifika tend to become infected with a more carcinogenic strain of H. pylori, further contributing to the heightened risk of stomach cancer.”
Kate says H. pylori infection is widely recognised to be the most significant risk factor in whether stomach cancer develops.
“The best way to prevent stomach cancer is to stop the infection in its tracks as early as possible with antibiotics. However, H. pylori is becoming more resistant to antibiotics limiting clinicians’ ability to eradicate this bacterium.”
If someone is infected with a strain that is resistant to the prescribed antibiotics , clinicians fail to eradicate H. pylori and the patient has a higher risk of developing stomach cancer.
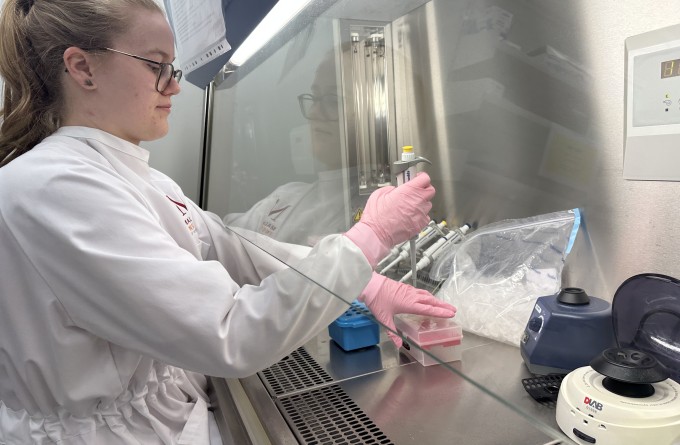
The research involves extracting H. pylori DNA from patient samples, detecting the presence of antibiotic resistance genes, and tailoring antibiotic therapy based on the resistance profile. The aim is to prescribe the right antibiotic for the right person. This will increase successful eradication, reduce inappropriate prescribing of antibiotics, and hopefully reduce rates of stomach cancer in Aotearoa New Zealand.
Kate and her team hope this transformative approach to the treatment of H. pylori could be implemented into Aotearoa’s healthcare system as a preventative measure for stomach cancer.
“It’s really important to me that this research could help address the inequities that exist in our healthcare system.”
Kate’s interest in science stems for her childhood growing up on farm in Omakau, Central Otago.
“I’d watch my dad with fascination as he bred sheep. He would take me through the genetics of the process. I was convinced that I wanted to be a vet.”
By the time she went to the University of Otago for her undergraduate degree, her focus had shifted to human biology and she chose to study health sciences, getting her undergraduate degree in Medical Laboratory Science.
“I was more interested in how things work rather than actually practicing it so I decided to pursue a more research-based career.”
She worked in a hospital diagnostics lab in Dunedin for a few years before moving to Wellington in late 2020 to work as a research officer in the Malaghan Institute’s hookworm programme.
“My grandma has colitis and my Mum has lupus so I’ve seen first-hand the effects these diseases can have on people and their families. That’s why the hookworm research intrigued me so much,” says Kate.
Kate is excited to apply what she’s learned over the last three years on a different area of research.
“I’m very happy to start working on a project which will have a direct benefit for people in New Zealand and could pave way for reducing the rates of stomach cancer,” says Kate.
“It’s really important to me that this research could help address the inequities that exist in our healthcare system.”
Related articles
In Focus: Mapping the lung's fight – how the entire organ responds to infection
18 April 2024

In Focus: Shooting for the stars, propelling our research in the information age
21 March 2024
In Focus: Tailoring mRNA vaccines for immunocompromised populations
14 December 2023
In Focus: A gateway for toxic damage and immune health
9 November 2023
In Focus: Mastering the technology behind automated CAR T-cell manufacture
14 September 2023
In Focus: Using state-of-the-art technology to probe the immune system’s role in health and disease.
9 August 2023
