Immunotherapy is fundamentally changing cancer treatment. By harnessing the power of the immune system, we’re finding new ways to assist or train the immune system to better recognise and fight different forms of cancer to create gentler, more effective treatments.
Our research focuses on developing therapies that stimulate the immune system’s cancer-killing properties.
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues. Cells can become cancerous for a number of reasons, whether through a mutation or by damage to a cell’s DNA from an outside source such as radiation. A large part of the immune system is dedicated to finding and removing these cells before they spread. A cancerous cell might look different to a healthy cell, or produce abnormal signals that alert patrolling immune cells to its presence.
However, sometimes the immune system fails to properly recognise, or completely remove all the cancerous cells. Many cancers develop ways to avoid detection by the immune system, hiding ‘in plain sight’ to appear as a normal, healthy cell. Some tumours can even produce immune-inhibiting molecules, preventing immune cells from reaching the cancer.
While these challenges make treating cancer difficult, they provide opportunities for developing immunotherapies to help the immune system better recognise and fight many different forms of cancer.
Our research also focuses on the underlying biology of cancer cells and the immune cells responsible for detecting and removing them. Through better understanding of cancer, tumours and the immune system, we can identify new opportunities to target cancer and improve cancer immunotherapies.
Associated research groups
Related News

Significant milestone reached in first NZ CAR T-cell trial as preparations made for larger phase 2 registration trial
25 March 2024
RNZ: Engineering immune cells to kill cancer
5 November 2023

BioOra appoints CAR T-cell therapy pioneer, Professor Carl June to Board
31 October 2023
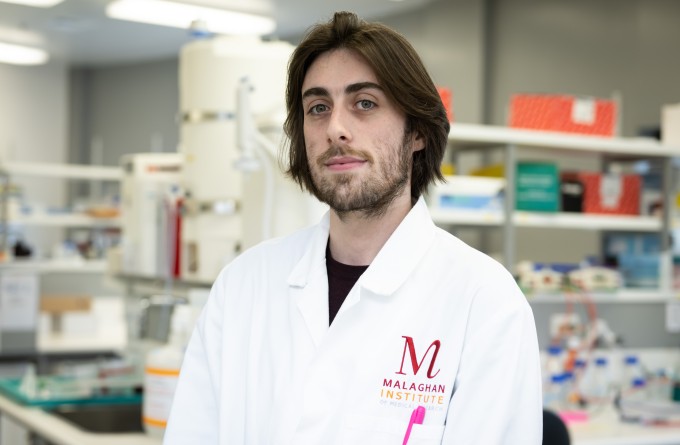
In Focus: Mastering the technology behind automated CAR T-cell manufacture
14 September 2023

RNZ: New Zealand developed cancer treatment one step closer to market
17 May 2023

Malaghan PhD student receives Māori Cancer Researcher Award
28 April 2023
