16 January 2023
Dr Olivier Lamiable is a team leader at the Malaghan Institute using revolutionary CRISPR-Cas9 technology to understand how allergic diseases develop on a cellular and molecular level.
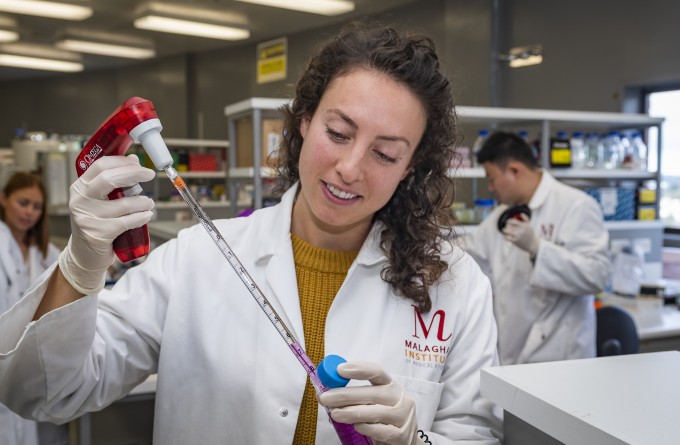
CRISPR-Cas9 is an exciting addition to the Malaghan Institute’s repertoire of tools to investigate the immune system.
“There will always be new technologies that allow you to expand your research or even unlock knowledge that we had no way of accessing previously. CRISPR-Cas9 is one of those technologies,” says Olivier.
“It allows us to precisely modify, add or remove specific parts of the DNA of live cells in a way that is faster and easier than any method before.”
Olivier is a member of the Ronchese Laboratory at the Malaghan Institute, a group focused on investigating the fundamental biology behind the development of allergies and inflammatory conditions.
“When I started working on dendritic cells in the Ronchese Lab, one of my goals was to implement this technology in the institute.”
“My son has allergies as do many other kids at his school. This isn’t how it should be and it’s not how it used to be.”
Specifically, Olivier is trying to understand which genes are involved in the function of a molecule called CCL17 which might be involved in conditioning T-cells to react and drive allergic responses.
“CCL17 is secreted by dendritic cells, the messenger cell which first presents a fragment of the allergen to the T-cells,” says Olivier.
“Using CRISR-Cas9, we can precisely stop the function of several genes that regulate CCL17 including genes that code for receptors and signalling molecules to find out how these genes are controlling the expression of CCL17.”
Since CCL17 activity is so important during allergic immune responses, finding which genes can be tweaked to stop its expression maybe give us better insight into how to stop developing allergies.
The ability to precisely edit the genes of live cells may sound like science fiction. In fact, CRISPR-Cas9 made shockwaves when it was first discovered. This mechanism, for decades obscured in the niche area of bacterial immunology, was found to have profound applications across biological and medical research as well as a potential therapy for genetic diseases.
The technology repurposes an ancient mechanism which is part of the bacterial immune system. Bacteria have had to develop protection against viruses which have been infecting them for as long as they’ve existed – more than 3.5 billion years.
"When a virus infects a bacterium, it can result in the bacteria dying. If the bacterium survives however, it remembers the viral infection and stores a piece of the virus in its DNA.”
Bacteria incorporate a piece of viral DNA into their own DNA and pass it on to future descendants. This piece of viral DNA is used as a surveillance system to protect against viral threats in the future. As a result, there are whole sections in bacterial DNA which contain the history of the viral infections of their ancestors, like a historical reference library full of past foes. These viral sequences are called CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats).
Bacteria use CRISPR to make RNA molecules containing the historic viral sequence.
“This RNA molecule, with the help of a protein called Cas-9, patrols the bacterial cell looking for any DNA that matches this sequence,” says Olivier.
If a match is found, it is assumed that the virus has come back to invade the bacteria. Without wasting any time, the Cas-9 makes two precise snips on either side of the viral DNA, destroying the invading virus.
When using CRISPR-Cas9 in the lab, researchers can design the exact sequence they want to target and make an RNA molecule that corresponds to this sequence. They can then equip the Cas9 protein to either cut either side of that sequence or tweak it further to add the sequence to that part of the DNA.
“As a geneticist, CRISPR is a fantastic tool to perform genetic analysis that has pushed the boundaries of what was thought possible,” says Olivier.
“It’s great to be a part of a global endeavour to answer the fundamental questions of how life works.”
Applying CRISPR-Cas9 to understand how allergic diseases develop could help determine which genes are involved in priming the cells that are activated during allergic disease.
“Currently, the treatments we have for allergic diseases mainly address the symptoms of allergic diseases rather than the cause,” says Olivier.
“Recently developed class of treatments such as biologics and jakinibs can address allergic disease slightly earlier in the process but still does not cure you of the allergic disease.”
The closest treatment we have to an allergy cure is desensitisation whereby the patient is gradually exposed to more and more of the allergen until their body becomes more tolerant of it.
“This is effective in patients but is still not completely efficacious in most people. Our ultimate goal is to find new ways of treating allergies that actually cure the allergy itself or try to prevent it from developing in the first place,” says Olivier.
“My motivation comes from helping people. I’m very aware of the growing problem that allergies pose. My son has allergies as do many other kids at his school. This isn’t how it should be and it’s not how it used to be. I want to find answers to why this is happening and how we can prevent this from happening.”
Olivier has been working at the Malaghan Institute for almost six years. Growing up in Orléans, France, he undertook his undergraduate and PhD at Université d'Orléans before moving to Strasbourg in 2011 for his first postdoctoral position at the Université de Strasbourg. He was there when the head of the lab, Professor Jules Hoffman, received a Nobel Prize for his discoveries on how the immune system detects microorganisms.
“It was very interesting to experience the very sudden media interest in the field and lab I was working in.” says Olivier.
“It’s great to be a part of a global endeavour to answer the fundamental questions of how life works. Technologies such as CRISPR-Cas9 are just one of many to come that will allow us to get more answers and reveal even more questions that we need to answer.”
Related articles
New research deepening understanding of elusive eosinophils
27 June 2024

International collaboration finds lipid imbalance in the skin may contribute to inflammatory conditions
24 June 2024
Double doctor: exceptional thesis awarded to Malaghan gastroenterologist
5 June 2024
Location, location, location: study finds where MAIT cells live may determine their role in allergic disease
12 February 2024
Health Research Council to fund clinical study investigating the skin’s role in initiating allergic disease
28 June 2023
In Focus: From tiger conservation to parasites and the allergy epidemic
10 May 2023
