3 November 2023
New Zealand’s first trial of a ground-breaking cancer treatment called CAR T-cell therapy has shown the promise of being safer than leading commercial CAR T-cell products in treating certain types of blood cancer, while remaining effective.

The Malaghan Institute ENABLE CAR T-cell clinical team
The Malaghan Institute’s ENABLE phase 1 safety trial began in late 2019, in partnership with Wellington Zhaotai Therapies Ltd, treating 21 New Zealanders with relapsed or refractory B-cell non-Hodgkin lymphoma who had exhausted all conventional treatment options. Participants received an experimental form of a novel ‘third generation’ CAR T-cell therapy at increasing doses, primarily to test the safety of the therapy. The trial was conducted with the support of Te Whatu Ora – Health New Zealand.

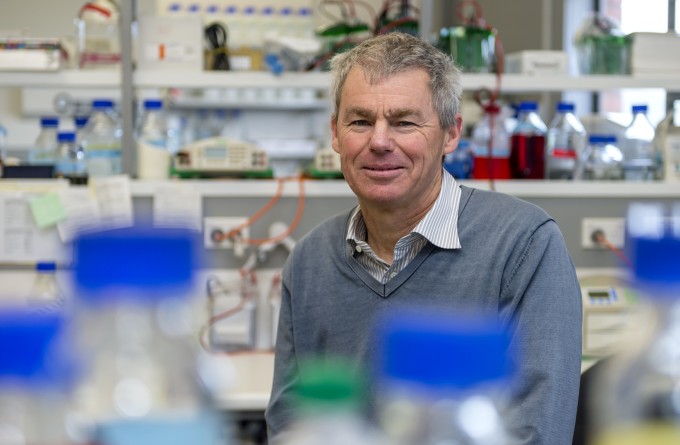
Clinical Director Dr Rob Weinkove
Preliminary results were published online today in an abstract accepted for presentation at the American Society of Hematology (ASH) Annual Meeting in San Diego. The trial found no limiting toxicities at any of the doses tested. Importantly, none of the participants developed neurotoxicity or severe cytokine release syndrome – common side effects of some commercial CAR T-cell therapies. The trial also showed promising effectiveness, with around half of the participants’ lymphomas in complete response three months after receiving the treatment.
“These results suggest our new CAR T-cell therapy may reduce risk of severe side effects, while remaining effective,” says Malaghan Institute Clinical Director Dr Rob Weinkove. “We are preparing for a larger trial to confirm this.”
The CAR T-cells were manufactured from participants’ own immune cells at the Malaghan Institute of Medical Research, with the treatment administered at Te Whatu Ora Capital, Coast and Hutt Valley.
“It’s fantastic to show that we can do this in New Zealand,” says Dr Weinkove. “This is a hugely ambitious clinical trial proving we can conduct cutting-edge trials that draw international attention.
“Even more importantly, it demonstrates that we can develop high-tech manufacturing here in New Zealand, and that there are no insurmountable obstacles to delivering new cancer treatments like CAR T-cell therapy in our hospitals.”
CAR T-cell therapy works by separating a patient’s own immune cells (T-cells) from their blood, and modifying them by introducing a new genetic sequence. The T-cells then make surface receptors called CARs which enable the T-cells, now CAR T-cells, to identify and attack the patient’s cancer.
“It’s fantastic to show that we can do this in New Zealand. This is a hugely ambitious clinical trial proving we can conduct cutting-edge trials that draw international attention."
Like building blocks, CARs are made of distinct subunits or domains made out of proteins. Each domain plays a different role that works together to help the T-cell find and kill a cancerous cell. The Malaghan Institute’s CAR T-cells include an additional ‘TLR2’ domain which Dr Weinkove and his team believe has helped make them safer.
“Our CAR T-cell product shares one of its domains with commercial CAR T-cell therapies called axi-cel (Yescarta) and brexu-cel (Tecartus). Axi-cel and brexu-cel are very effective treatments, but neurotoxicity affects up to half of recipients. We think that adding the new TLR2 domain in our construct has lowered the neurotoxicity rate, hopefully while maintaining effectiveness,” he says.
“Our laboratory research programme, supported by Freemasons New Zealand, suggests that our CAR T-cell product has a low risk of neurotoxicity because the new TLR2 domain has changed levels of the chemicals or ‘cytokines’ that can drive inflammation in the brain. Apart from the direct benefit to patients, a low neurotoxicity rate means that we can treat patients without routinely admitting them to hospital for monitoring, lowering costs for the health system.”
The next phase of this programme is to improve the manufacture and delivery of CAR T-cells using cutting-edge automation technology. “We are already treating patients in an ‘expansion cohort’, for which we have automated the CAR T-cell manufacturing process with our partners at BioOra, and we are giving the CAR T-cells as an outpatient therapy,” says Dr Weinkove.
“This cohort is helping us prepare for a phase 2 trial, in which we would like to treat a larger number of people across New Zealand, to learn exactly how effective our treatment is, and to get more information about side effect rates.”
As a phase 1 safety trial, patients could only enrol to the ENABLE trial after they had exhausted all other treatment options, says Dr Weinkove.
“This is difficult, because people often have side effects from their prior chemotherapies, such as low blood counts or kidney damage, and because if their lymphoma progresses while we are making their CAR T-cells, we have limited options to control the disease. Because the toxicity rates are low in the phase 1 trial, we aim to treat patients earlier in their treatment pathway in a phase 2 trial.
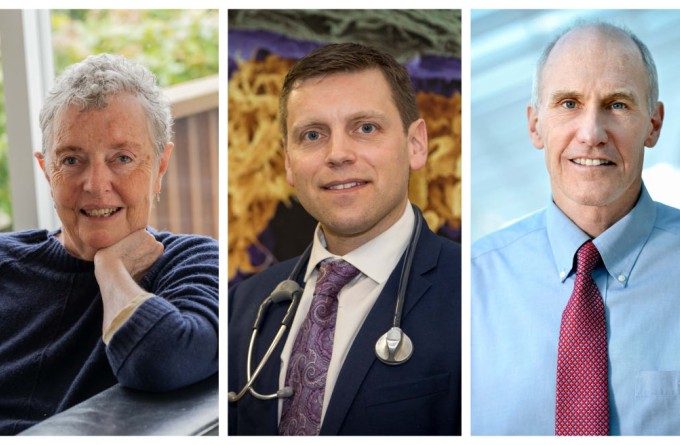
Dr Carl June, Richard W Vague Professor in Immunotherapy at the University of Pennsylvania and BioOra board member, recognised as a pioneer of CAR T-cell therapy, says the ENABLE trial’s phase 1 CAR T data to be presented at ASH are a step forward for the treatment of CD19-expressing lymphomas.
“Dr Weinkove and his team at the Malaghan Institute and BioOra have shown efficacy that is on par with commercial CAR T, but the safety signal appears superior. This lays the foundation for outpatient delivery and management and expanding indications of their CAR T programme.”
Dr Weinkove says the team here in New Zealand has taken this process all the way from developing a new CAR T-cell manufacturing process, establishing clinical and safety procedures, and treating and following-up patients. Their ultimate goal is to make CAR T-cell therapy a standard of care in New Zealand hospitals.
“We are hugely grateful to the patients who have taken part and to their whānau, and for the Malaghan Institute’s many supporters.”

The ENABLE trial was funded by the Ministry of Business, Innovation and Employment, Thompson Family Foundation, and by private donors, with additional support from Leukaemia & Blood Cancer New Zealand and Life Blood. The Malaghan Institute's CAR T-cell research programme has been supported by Freemasons NZ and the Health Research Council of New Zealand. Dr Weinkove received a Clinical Practitioners Research Fellowship from the Health Research Council.
Related articles

Phase 2 clinical trial underway to confirm effectiveness and safety of NZ’s first CAR T-cell cancer therapy
23 July 2024
CAR T-cells approved by EPA for phase 2 trial
23 May 2024
A revolution in cancer care is near; here’s what’s needed to make it happen
9 May 2024

Significant milestone reached in first NZ CAR T-cell trial as preparations made for larger phase 2 registration trial
25 March 2024
Freemasons New Zealand renews support for CAR T-cell therapy
10 November 2023
RNZ: Engineering immune cells to kill cancer
5 November 2023
