7 November 2022
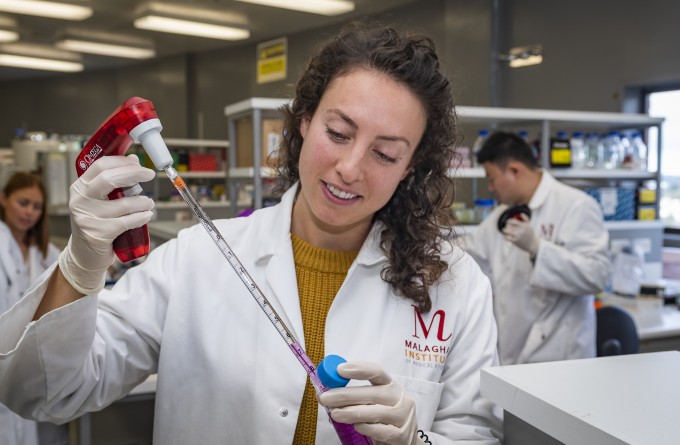
A study by the Le Gros Laboratory at the Malaghan Institute has uncovered genetic clues that help explain how certain immune cells can cause allergic disease. The paper, published in Immunology and Cell Biology, brings us one step closer to preventing the cellular mechanisms that drive the development of allergic and inflammatory diseases by targeting the specific immune cells that trigger them.

Professor Graham Le Gros and Dr Jodie Chandler
Allergies and autoimmune conditions are caused by immune cells mistakenly labelling harmless materials, such as food, pet dander or even healthy tissue, as dangerous or life-threatening. Responding to the perceived attack as real, the resulting immune response can range from a light rash to anaphylactic shock. What causes specific immune cells to trigger allergic and inflammatory responses and whether we can design therapies to prevent this from happening is a key area of research for scientists like Dr Jodie Chandler who completed her PhD in the Le Gros lab.
“There is still a lot we don’t understand about the genetic and physiological changes in immune cells that nudge the immune system towards an allergic response,” says Dr Chandler, “which is why basic or fundamental research on the immune system is so important.”
Different immune cells play different roles in the many thousands of responses the immune system performs every day. In this study, the Le Gros lab focused on one key type of immune cell they believe plays a leading role in driving pro-allergic responses.
“Our research focussed on a specific type of T-cell called a T-follicular helper cell (Tfh),” says Dr Chandler. “Tfh cells play a critical role in the body where they help B-cells to activate and start producing antibodies. Without Tfhs we wouldn’t get effective antibody production, which is critical to help combat diseases!”
In an allergic setting, Tfh cells help generate a specific antibody that binds to immune cells that trigger the release of histamines, causing classic allergic symptoms that are typically combatted with anti-histamines.
“We know Tfh already play an important role in allergic responses, but we wanted to better understand how Tfh cells develop in the body and whether they retain a level of plasticity that would enable them to further develop into other types of T-cells and drive allergic symptoms beyond their Tfh/B-cell antibody interaction.
“Specifically, we wanted to know if Tfh cells can develop into type 2 helper T-cells (Th2) that play a pivotal role in allergic diseases. Understanding what makes a Th2 cell a Th2 cell is an important part of developing strategies to prevent them promoting allergic disease.”
Th2 cells are strongly linked to the development of allergic diseases such as asthma or eczema. They are triggered when exposed to specific allergens and initiate dangerous inflammation in the body.
“We found that when we delete Tfh cells in animal models we still see Th2 cells present in the skin, driving allergic disease. This indicated that no, Tfh cells do not further develop into Th2 cells – at least in the skin. – implying they’re originating from somewhere else in the body,” says Dr Chandler.
“While this isn’t a smoking gun from a disease standpoint, our findings are important as the more we know about Th2 development, and what drives their development, the more potential pathways we have to disrupt the mechanisms that promote allergic disease.”
Related articles
New research deepening understanding of elusive eosinophils
27 June 2024

International collaboration finds lipid imbalance in the skin may contribute to inflammatory conditions
24 June 2024
Double doctor: exceptional thesis awarded to Malaghan gastroenterologist
5 June 2024
Location, location, location: study finds where MAIT cells live may determine their role in allergic disease
12 February 2024
Health Research Council to fund clinical study investigating the skin’s role in initiating allergic disease
28 June 2023
In Focus: From tiger conservation to parasites and the allergy epidemic
10 May 2023
