3 May 2021
The gut holds a unique position in the body, serving as the interchange between our external environment (via the food we eat), the billions of microbes that call it home, and our immune system. Over 70% of our immune system is located in the gut, but we are only just beginning to understand the depth of its influence. Given its enormous complexity, it’s unsurprising that uncovering meaningful information from the gut – especially how it influences human health – is like looking for a needle in a haystack.

“The gut is a complex and multi-faceted organ with many different functions,” says Malaghan Institute Director Professor Graham Le Gros. “It’s difficult to probe and to analyse, and it can only truly be understood by looking at the wider context of the microbiome, the biochemistry of food and the function of immune cells. And that’s exactly what we’re doing.”
The Malaghan Institute has been steadily pooling expertise from different disciplines – bringing together a world-leading superteam across metabolics, immunology, nutrition and physiology – for a more holistic and comprehensive view of the immune system and the gut.
And thanks to recent advancements in analytical technology, and the ability to process billions of cells in a short space of time, the Institute’s scientists can now investigate some of the big questions about the relationship between our gut, our immune system and our health.
Feeding our gut and the microbes that call it home
We are what we eat, but also, we are our microbes. The gut is responsible for taking the food we eat and turning it into fuel to power our cells. But on their own, our bodies can’t break down food into useable components – or ‘metabolites’ – we rely on the billions of bacteria that live in our gut, otherwise called the microbiome. Our immune system regulates the microbiome, and in turn is influenced by the types of metabolites produced by the microbiome – a feedback loop that affects not just the health of our gut, but of the rest of our body too.
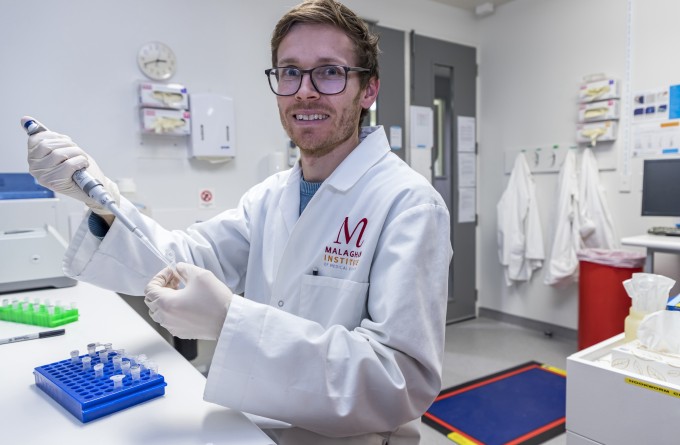
To tackle how diet and the microbiome affect our metabolic health, Dr Olivier Gasser and his Translational Immunology team have several ongoing research projects, investigating how metabolites generated by the microbiome spread throughout the body and influence the behaviour of immune cells in the brain, lung and skin. By better understanding what metabolites and microbes contribute to a healthy immune system, we can then determine whether we can improve things like immune responses to vaccines through certain dietary manipulations.
Understanding the role of immune system in the gut
A healthy immune system means a healthy gut, which in turn benefits the rest of the body. When things go awry, or the immune system is not doing its job, we want to know what led to this imbalance, and whether we can use diet, microbes – or a combination – to steer the immune system back on course.
To understand how to improve a troubled immune system in the gut, we must understand what a ‘healthy’ immune system looks like. One of the overarching goals of our therapeutic hookworm programme is to use parasites to teach us how a healthy immune system adapts and responds to a harmless infection. By quantifying how the immune system responds to a parasite, especially at the site of infection in the gut, we can then take this data and apply it in the context of inflammatory diseases.
We also know that many immune disorders have their origins in the gut. So we’re using cutting-edge bioinformatic and gene sequencing techniques to track various immune cells as they develop, to help identify what the root causes are that nudge these cells towards causing disease.
From the lab to the clinic
When dealing with the complexity of gut-health interactions, fundamental laboratory research can only go so far. The best way to understand the gut in the context of human health is in a clinical setting.
The Malaghan Institute recently recruited gastroenterologist Dr Tom Mules to bridge the gap between laboratory and clinical work.
“Tom plays a key role in our gut health programme – as the clinical link helping us run clinical trials and studies focusing on the gut,” says Prof Le Gros. “As a clinician, he is an expert in the physiology of the gut, and is well placed to help us understand how different components of the gut may be influencing different aspects of immune-related disorders such as ulcerative colitis and inflammatory bowel disease.”

Dr Tom Mules
Related articles

Dr Michelle Linterman: Asking the age-old question
30 April 2025
Fever: too hot to handle or the body's first line of defence?
22 August 2024
RNZ Our Changing World: Targeting bacteria, and health inequities
4 July 2024
New research deepening understanding of elusive eosinophils
27 June 2024
Double doctor: exceptional thesis awarded to Malaghan gastroenterologist
5 June 2024
New clinical research aims to reduce stomach cancer rates and disparities in New Zealand
28 May 2024
