28 May 2024
A new clinical research programme which aims to increase the successful eradication of Helicobacter pylori (H. pylori), a bacterium that lives in the stomach and is the leading cause of stomach cancer, has been awarded a $150,000 Explorer Grant from the Health Research Council of New Zealand.

H.pylori and stomach cancer disproportionately impact Māori and Pacific peoples in Aotearoa New Zealand. When H. pylori is identified and treated, stomach cancer can be prevented. However, the ability to successfully treat and eradicate H. pylori with commonly used antibiotics is declining due to increasing antibiotic resistance.
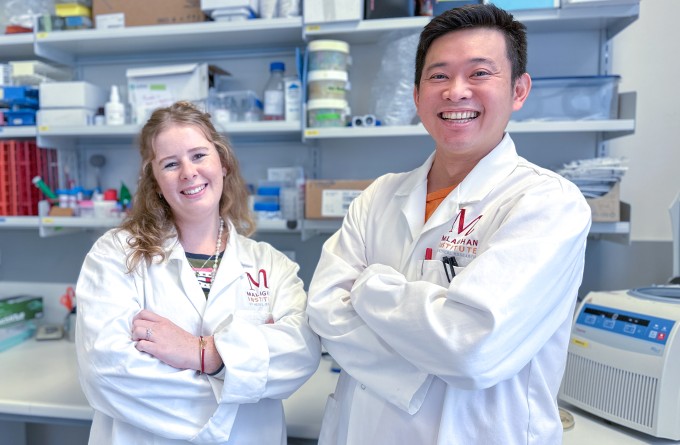
Dr Tom Mules and Dr Stephen Inns, gastroenterologists at Te Whatu Ora Hutt Valley and clinical researchers at the Malaghan Institute of Medical Research and the University of Otago, respectively, are developing and validating new methods to test for antibiotic resistance in H. pylori to guide antibiotic prescribing.
H.pylori is responsible for most stomach cancers in New Zealand. Usually contracted in childhood, H. pylori infects the cells of the stomach, causing gastritis, or inflammation of the stomach lining. Left untreated, the inflammation can become chronic leading to tissue damage and ulcers and eventually, cancer.
“The best way to prevent stomach cancer is to eradicate H. pylori,” says Dr Mules. “However, H. pylori is becoming more resistant to antibiotics, limiting our ability to treat infections.”
In New Zealand, the current practice is to prescribe everyone the same antibiotics to treat H. pylori,without knowing if it is the right antibiotic regimen for that individual.
“By determining the antibiotic resistance profile of H. pylori, we aim to individualise treatment regimens to increase eradication and decrease inappropriate antibiotic prescribing,” Dr Mules says.
Significant disparities exist in the rates of stomach cancer among Māori and Pacific populations in Aotearoa, who have three to six times higher rates compared to New Zealand Europeans according to a University of Otago study.
“These ethnic inequalities in stomach cancer rates predominantly stem from the higher prevalence of H. pylori infection among Māori and Pasifika,” says Dr Mules. “Māori and Pasifika are also more likely to be infected with a more carcinogenic strain of H. pylori, further contributing to the heightened risk of stomach cancer.”
The research involves extracting H. pylori DNA from patient gastric tissue samples or stool samples taken as part of routine clinical testing for the presence of H. pylori, analysing these samples for the presence of antibiotic resistance genes, and tailoring antibiotic therapy based on this gene profile.
“Being able to individualise treatment so we can prescribe the right antibiotic for the right person is crucial to improve treatment success, while also reducing inappropriate antibiotic prescribing,” says Dr Mules.
Taking place at Hutt Hospital, the first phase of the research programme is already underway.
Dr Mules says the next phase is to perform a clinical trial to determine if routinely testing H. pylori for the presence of antibiotic resistance, and then individualising therapy based on this result, will increase the effectiveness of treatment in the clinical setting.
“This research has the potential to profoundly transform clinical practice, directly addressing and rectifying significant healthcare equity concerns in Aotearoa New Zealand.”
RELATED ARTICLES

Malaghan CAR T-cell cancer therapy trial expands to Christchurch and Auckland
23 June 2025
Research sheds new light on the allergic response – and how to disrupt it
5 June 2025

Horizontal mitochondria transfer: 10 years on from a groundbreaking discovery
7 May 2025

Kjesten Wiig: bringing life-changing treatments to life
27 February 2025

Cancer Research Trust grant to improve CAR T-cell therapy
12 February 2025

World-renowned cancer pathologist joins the Malaghan Institute as Distinguished Research Fellow
19 December 2024
