3 May 2021
With the astronomical success of CAR T-cell therapy, it’s hard to believe that this groundbreaking cancer treatment is still in its infancy. Just as the first automobiles bear little resemblance to today’s cars, CAR T-cell technology has much room for improvement, despite already saving many lives around the world.

Here in New Zealand, our ENABLE phase I clinical trial involves ‘third generation’ CAR T-cells – the third iteration of this novel technology – with second generation CAR T-cells licensed for use in places like Europe, the United States and Australia. The hope is that third and subsequent generations of CARs build and improve upon this treatment with fewer toxicities and side effects. Clinical Director Dr Rob Weinkove explains:
“The term ‘third generation’ relates to the structure of the ‘CAR’ – the receptor that makes CAR T-cells work. Developed in the late 1980s, first generation CAR T-cells sent only one type of signal (or alert) when they encountered a tumour cell, and they did not effectively eradicate the tumours. By the 2010s, second generation CAR T-cells provided two types of signal to the T-cells, improving the CAR T-cells ability to kill tumour cells. In 2018, several second generation CAR T-cell products were licensed for use by the US Food and Drug Administration. However, while many recipients fare well, at present, most patients with aggressive B-cell lymphomas, myeloma and B-cell acute leukaemias relapse after receiving second generation CAR T-cell therapies, indicating the need for further improvements.
“Building on the second generation versions, third generation CAR T-cells have three portions within the CAR that signal to the T-cell to kill its target. Several third generation CAR T-cells are in clinical trials, including ours.”

The third generation CARs in development around the world all use different types of signals, trying to determine which one(s) have the best results. At the Malaghan Institute, our third generation CARs – developed in partnership with Wellington Zhaotai Therapies – use a unique signal we hope will make the therapy more effective.
“This additional signalling domain emulates a ‘danger’ signal, effectively making the CAR T-cells act as if they are seeing a bacterial infection,” says Dr Weinkove. “This unique domain adds to the effectiveness of CAR T-cells in laboratory models, and our current trial programme is assessing if this addition is both safe and effective in patients.”
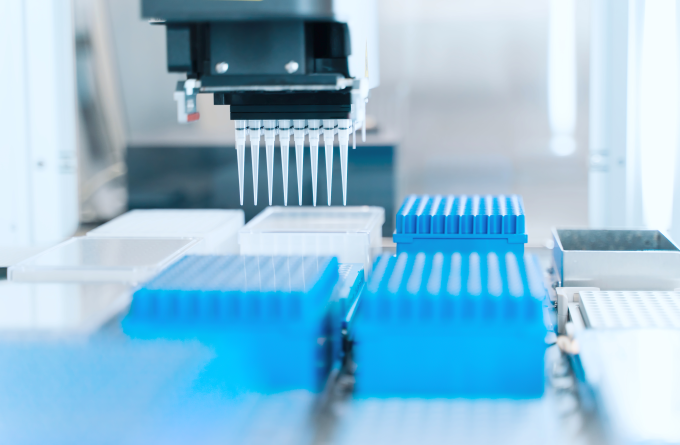
While the ENABLE trial is still underway, Dr Weinkove and the rest of the Freemasons CAR T-cell Research Programme are already finding new ways to improve on both the manufacture and delivery of CAR T-cells, and researching new kinds of CARs with better signalling and in-built ‘safety switches’ to rapidly deplete CAR T-cells should a patient experience negative side effects.
Related articles

Malaghan Institute becomes New Zealand’s first signatory to the Technician Commitment
11 July 2025

Malaghan CAR T-cell cancer therapy trial expands to Christchurch and Auckland
23 June 2025

Distinguished service award for head of Hugh Green Technology Centre
20 May 2025
Boost for medical research with new blood processing service for clinical trials at Malaghan
19 May 2025

Horizontal mitochondria transfer: 10 years on from a groundbreaking discovery
7 May 2025

Kjesten Wiig: bringing life-changing treatments to life
27 February 2025
