1 July 2020
How the immune system could be used to target the malaria-causing parasite plasmodium is part of a trans-Tasman project which has recently received nearly $1.2m funding from the Health Research Council of New Zealand.

Malaria is a global health issue that kills nearly half a million people each year according to the World Health Organization, with no effective long-term vaccines. The disease is caused by the plasmodium parasite that resides in the saliva glands of mosquitos and is transferred to humans when the mosquito feeds.
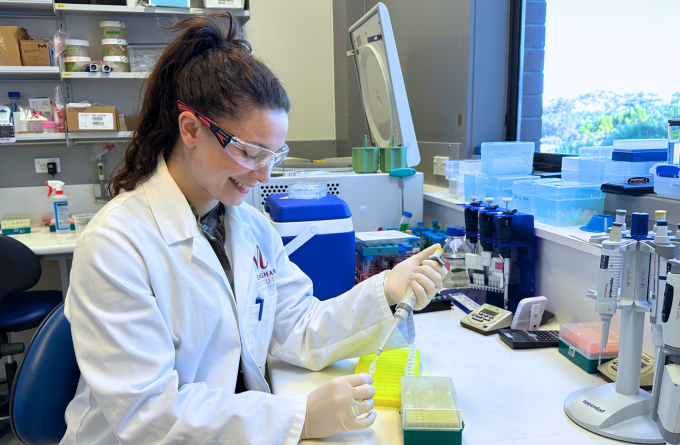
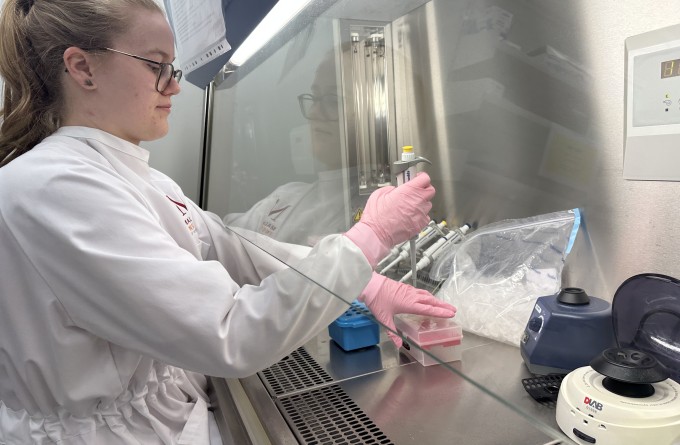
Alongside the Ferrier Research Institute, the University of Melbourne and Avalia Immunotherapies, the Malaghan Institute for Medical Research has been working over the past three years to develop a simple vaccine design that could be manufactured efficiently and administered easily in at-risk countries.
“Traditional vaccines typically work by looking for foreign bodies or antigens present on the surface of the pathogen,” says the Ferrier Research Institute's Professor Gavin Painter who is leading the HRC-funded project. “These antibody-producing vaccines can be incredibly potent and offer long-term immunity, however in the case of malaria they don’t work very well because the parasite resides inside cells that antibodies can’t reach.”
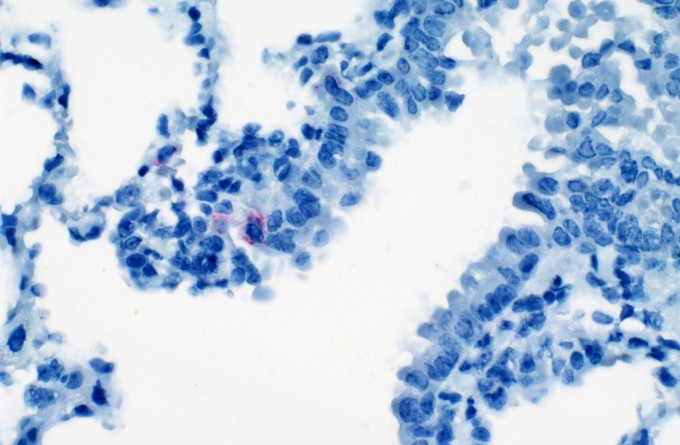
However, a crucial stage of the development of plasmodium occurs in the liver of infected humans, offering a potential inroad for developing a targeted immune response to this parasite.
“We know that our vaccine seems to create the right sort of environment to activate T-cells in the liver,” says the Malaghan Institute’s Deputy Director of Research Professor Ian Hermans. “When Prof William Heath at the University of Melbourne got wind of this he got really excited, as he’d been looking for ways to get a T-cell response in the liver for developing a protein-based malaria vaccine that targets the sporozoite stage of the plasmodium.”
Since then, Prof Heath has identified a host of plasmodium genes which may make good targets for a vaccine and has enlisted the Malaghan and Ferrier Institutes to help test them. The HRC-funded project, titled ‘Designing a scalable vaccine to induce liver resident T cells against malaria,’ will assess up to 38 gene candidates to determine which ones stimulate the best immune response in preclinical models.
“Right now, we’re taking a really broad approach to the question of how to create a malaria vaccine and trying to determine if it is feasible and what it might look like,” says Prof Hermans. “We’re a long way off human studies, but it’s a really unique way of creating a vaccine, which is why this trans-Tasman collaboration is so exciting.”
Related articles
In Focus: Mapping the lung's fight – how the entire organ responds to infection
18 April 2024

Malaghan and National Institutes of Health research receives prestigious award
5 March 2024
In Focus: Tailoring mRNA vaccines for immunocompromised populations
14 December 2023
Scientists identify interferon-gamma as potential SARS-CoV-2 antiviral
13 December 2023

New research suggests hookworms could offer protection from severe Covid symptoms
14 August 2023
Scientific breakthrough harnesses mRNA technology to develop powerful malaria vaccine
21 July 2023
