A revolutionary new approach to fighting cancer, CAR T-cell therapy has the potential to transform cancer treatment. We're working to make it accessible and affordable for all New Zealanders in need.
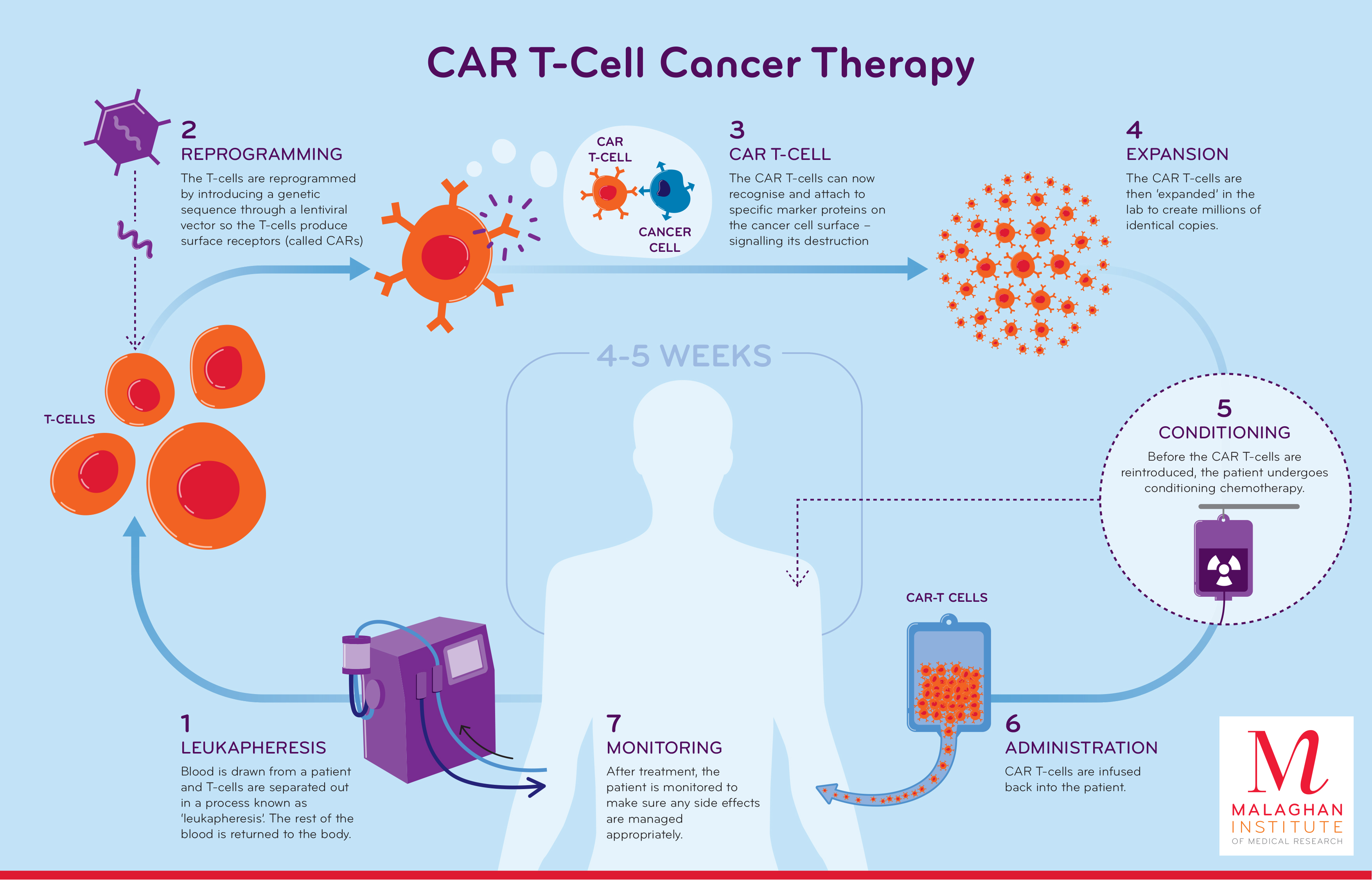
CAR T-cell therapy stands for Chimeric Antigen Receptor T-cell therapy. A one-off treatment, it works by redirecting a patient’s own immune cells (T-cells) in the laboratory, to directly identify and attack cancer cells. These modified T-cells are then returned to the patient where they can attack and destroy cancer cells. CAR T-cells have the potential to act as ‘living drugs’, providing long-term protection against relapse.
CAR T-cell therapy has the potential to target a range of cancers, with research and clinical trials underway worldwide. However, to date, it has been effective for treating certain blood cancers, including certain lymphomas, B-cell leukaemias, and myeloma. In Australia, the USA and parts of Europe, CAR T-cell therapies for these types of cancer are licensed for routine use.
In New Zealand, the Malaghan Institute’s CAR T-cell programme includes the country’s first CAR T-cell trial, with on-shore CAR T-cell manufacture and delivery. Our goals are to conduct cutting-edge trials of new CAR T-cell therapies, and to leverage our nationally-unique manufacturing, regulatory and clinical experience to help introduce CAR T-cell therapies as a standard of care in New Zealand.
ENABLE clinical trial
The Malaghan Institute, in partnership with Wellington Zhaotai Therapies, is developing and trialling a new CAR T-cell therapy in New Zealand for patients with certain types of relapsed and refractory B-cell non-Hodgkin lymphoma, who have exhausted other treatment options.
The treatment we are working on is a ‘third generation’ CAR T-cell therapy, which we hope may be at least as safe and effective, and easier to deliver, than treatments currently available elsewhere. Our ENABLE phase I safety trial got underway in late 2019, treating participants across the country to determine the optimal dose of the therapy. In January 2023 we treated our 21st and final patient in this dose escalation cohort.
Preliminary results of the trial, presented at the American Society of Hematology meeting in December 2023, found no limiting toxicities at any of the doses tested. Importantly, none of the participants developed neurotoxicity or severe cytokine release syndrome – common side effects of some commercial CAR T-cell therapies. The trial also showed promising effectiveness, with around half of the participants’ lymphomas in complete response three months after receiving the treatment – that is, no signs of cancer in the body.
These results suggest our new CAR T-cell therapy may reduce risk of severe side effects, while remaining effective.
Since then, a further nine patients have been treated at the optimal dose as part of a dose expansion cohort, with outpatient management and automated CAR T-cell manufacturing by our partners BioOra using Cocoon technology. Enrolment and treatment is now complete. Trial participants remain under follow-up, with a primary analysis of all 30 patients treated expected in June 2024, followed by publication of the results.
We are now preparing for a larger phase 2 registration trial, later in 2024, where effectiveness can be assessed more robustly. Because of the low toxicity rates in the phase 1 trial, we hope to treat patients earlier in their treatment pathway. The multi-site trial, ENABLE-2, will treat 60 patients over two years, with a view to regulatory approval.
The main barriers to CAR T-cell therapy globally are the burden of managing side effects and the cost of the CAR T-cells themselves. By combining an improved safety profile with cost-effective manufacturing, we aim to address both issues.
Trial recruitment
The Malaghan Institute is not a provider of health services and does not recruit patients to clinical trials directly. Patients should speak to their haematologist or oncologist about whether this, or other clinical trials, might be an option for them. Referrals must be made by a relevant specialist to the Clinical Trials Unit at Wellington Hospital via [email protected]. A public summary of the ENABLE trial is available on the ClinicalTrials.gov website.
CAR T-cell research programme
In parallel with the ENABLE clinical trial, our CAR T-cell research programme is focusing on improving the safety and effectiveness of current CAR T-cells, and expanding this cutting-edge technology to treat a wider range of cancers, including solid tumours.
ASSOCIATED RESEARCH GROUPS
Related News

Significant milestone reached in first NZ CAR T-cell trial as preparations made for larger phase 2 registration trial
25 March 2024
Location, location, location: study finds where MAIT cells live may determine their role in allergic disease
12 February 2024
Freemasons New Zealand renews support for CAR T-cell therapy
10 November 2023
RNZ: Engineering immune cells to kill cancer
5 November 2023

Trial results offer hope to Kiwis with incurable blood cancer
3 November 2023

BioOra appoints CAR T-cell therapy pioneer, Professor Carl June to Board
31 October 2023